Program Planning & Design
The literature on the practical aspects of planning and implementing community health worker programs is limited, but several detailed case studies highlight consistent best practices and lessons learned.
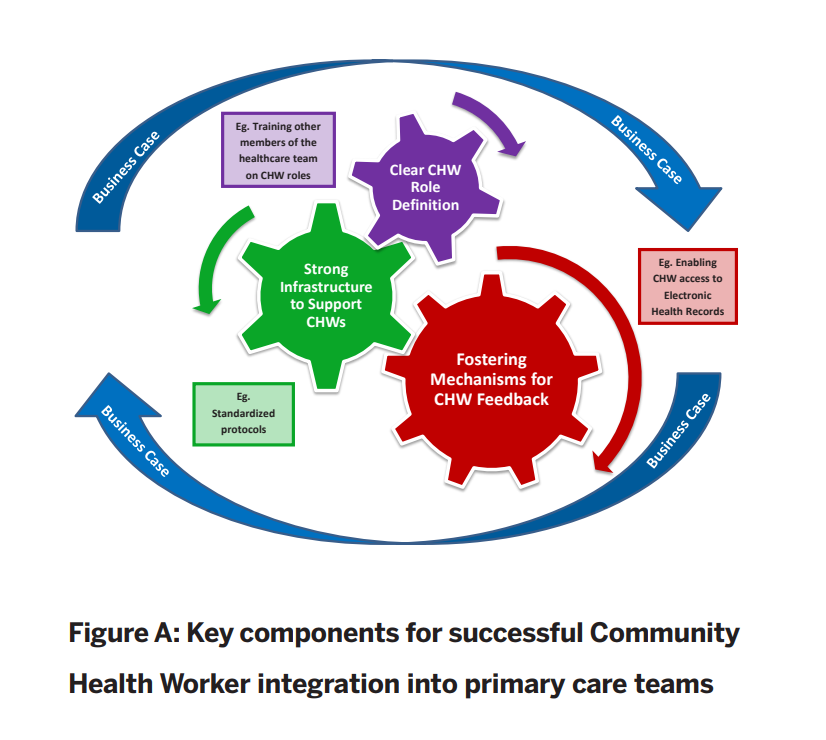
Source: Integration of Community Health Workers into Primary Care Systems
Lessons Learned in Operationalizing CHWs in Healthcare Teams
- Establish a community health worker job category in human resources. CHW job codes allow for appropriate job descriptions and support the advancement of CHWs. Job codes should maintain flexibility to facilitate community connection. (1)
- Create small CHW teams with a central manager. “Although CHWs may work in different geographies, the team structure allows for sharing of best practices and problem solving of difficult cases and also reduces the burden of compassion fatigue. Having a centralized manager protects the role of the CHW and prevents these employees from having to fill staffing gaps outside of their CHW responsibilities.” (1)
- Develop clear practice guidelines and protocols. “Clear information around caseloads, work flow, documenting, and supervision allow expectations to be understood by all invested parties. At times, CHWs encounter a patient with an urgent health need. Clear guidelines on timely reporting of these needs and to whom has been imperative to the safety of the CHW practice and the care of the patient. Standards of work practice has facilitated scaling the programs to other sites.” (1)
- Maximize community health workers’ time in community. At Bronx Lebanon PCMH, “almost half of CHW work is devoted to home visits, outreach and follow-up, with direct interactions with patients. These interactions allow CHWs to build a trusting relationship and teach self-care and disease management methods and support the patient’s progression toward achieving their disease management goals as established in their original visit with the CHW. All CHWs are expected to make 2 home visits per day and 3 joint clinic/hospital visits per day.” (2)
- Plan for CHW integration into care teams. One of the keys to success is “the commitment to continually improve the integration of CHWs as members of the care team. The department used many opportunities to help clinical staff to understand how CHWs were being integrated into the care team: Continuing Medical Education courses, rounds with CHWs, team meetings, staff meetings. Key was the participation of the CHW in routine monthly clinic team meetings… Community health workers presented detailed patient care narratives focusing on cultural, social, and communication issues. Other team members came to understand and appreciate that CHWs can discover information about the real circumstances of patients’ lives that patients do not readily share with other members of the team. The aim was for the CHW to be a full member of the medical team, not a secondary member “as needed” or on referral.” (2)
Source 1: Integration of Community Health Workers into Primary Care Systems
Source 2: CHW Integration into a Healthcare Team: A Bronx Tale
Tools & Templates
The MN Community Health Worker Toolkit provides a detailed list and links to tools and templates to assist CHWs and their supervisors and care teams in the process of service delivery. These include:
- Policy and procedure manuals;
- Triage protocols;
- Patient assessment;
- Health promotion and patient education materials;
- Follow-up protocols and forms; and,
- Care coordination protocols and forms
Highlights include:
- Pathways Community HUB model which has developed 20 open source pathways for a variety of health and social issues;
- HealthEast Care System has provided a number of protocols for CHW integration into care teams, including EHR protocols and examples.
As stated in the MN Community Health Worker Toolkit “ideally, planning for cost-benefit analyses should be included in initial program planning. Estimated ROIs are beneficial for developing the business case, and advance planning ensures data is/are available and can be collected. A few templates and toolkits have been designed for conducting a cost-benefit analysis and are described below:
- ROI Toolkit: A Guide for Conducting a Return on Investment Analysis of Your Community Health Worker Program. Developed by MHP Salud in Texas with funding from Health Resources Services Administration (HRSA), the toolkit is a practical, step-by-step guide for planning and implementing a ROI analysis. Designed specifically for community or clinical CHW programs, the guide includes many sample data sources and some templates. The toolkit can be accessed by registering at the MHP Salud site.
- The ROI Calculator for Health Homes and Medical Homes and ROI Calculator for Other Quality Initiatives were both developed by the Center for Health Care Strategies, Inc. While not specific to CHW programs, both provide extensive Excel-based templates for analysis of ROI data. An instruction manual is included with the templates.
- There are also disease-specific templates including Building the Business Case for Diabetes Self-Management: A Handbook for Program Managers that may provide some additional ideas for conceptualizing ROI for CHW programs.
Some factors to consider when planning cost-benefit analyses include:
- Research questions – are the research questions the right questions?
- Indicators – do the indicators sufficiently measure and provide answers to the research questions?
- HIPAA – is the data collection in line with HIPAA requirements?
- Time – is the data collection period long enough to allow for relevant costs and to show a change?
- IRB– if performing research on individuals, institutional review board approval is typically required up-front.”
Example: In CHW Integration into a Healthcare Team: A Bronx Tale, “community health workers contributed substantially to improvements in care team productivity and outcomes.
- ED visits declined by 5.0%
- Hospitalizations by 12.6% among patients with diabetes and other chronic health problems.
- Community health workers generated a net savings of $1135 per patient, with each CHW generating a net savings of $170213 per year.
- The return on investment was 2.3, meaning that for every dollar invested in the CHW program, the hospital saved $2.30.
Results were shared among the care team members, hospital administration, and other hospital leaders, to publicize the value of CHW contributions. In addition, the Departmental Chair routinely reports CHW program outcomes to Healthcare Effectiveness Data and Information Set, Healthcare Services & Capital and other monitoring agencies.”
The CDC recommends that states “allow and promote CHW access to EHR systems to facilitate follow-up with patients, communication with providers on the care team, and patient referrals to community resources” in its Technical Assistance Guide for States Implementing Community Health Worker Strategies.
Best Practice Recommendations
- Develop an efficient referral system thru EHR
- Track high risk patients
- Create structured data fields for CHWs
- Allow CHWs access to hospital EHR for outpatient follow-up after hospital discharge
- Use mobile technology
Adapted from: Integration of Community Health Workers into Primary Care Systems and Integrating CHWs into a PCMH to Support Disease Self-Management Among Vietnamese Americans: Lessons Learned
A number of documentation and reporting tools are included in the MN Community Health Worker Toolkit. See Section 11.1.2 for a full list of EHR related templates.
Community Health Worker Encounter Forms: A Tool to Guide and Document Patient Visits and Worker Performance explores the effectiveness of using a CHW encounter form to collect data pertaining to patient interactions. It also assesses ways to use these forms to guide and direct interactions.
Community Health Workers and Mobile Technology: A Systematic Review of the Literature reviewed the evidence for the use of mobile technology by community health workers to identify opportunities and challenges for strengthening health systems in resource-constrained settings.
- Mobile technology for health data collection: “Most commonly, community health workers use mobile technology to collect field-based health data, receive alerts and reminders, facilitate health education sessions, and conduct person-to-person communication.”
- Mobile technology improves adherence: “Programmatic efforts to strengthen health service delivery focus on improving adherence to standards and guidelines, community education and training, and programmatic leadership and management practices. Those studies that evaluated program outcomes provided some evidence that mobile tools help community health workers to improve the quality of care provided, efficiency of services, and capacity for program monitoring.”
The following case examples of CHW use of mobile technology is described in Community Health Workers in an Evolving Technology Environment, National Partnership for Action to End Health Disparities.
- Care Navigator, developed by BluePrint Healthcare IT, allows community health workers to maximize their role in the community and as part of the care team by creating a platform that enables real time, team-based care coordination and communication. The Care Navigator strengthens the communication between the patient and provider and reinforces behaviors and strategies for health improvement based on the patient’s assessed needs.
- CommCare, developed by researchers from the University of Washington and the University of California at Berkeley, is a mobile phone-based software that aids CHWs in a variety of tasks including screening for illnesses such as TB and malaria, providing accurate information on family planning and safe drinking water, reminding patients about follow-up visits and keeping track of new births or deaths. Emerging educational applications of CommCare will enable CHWs to engage in refresher courses and continuing education to support continued effectiveness of CHWs.

